Nutritional Therapists should be in NHS Primary Care
As the National Health Service (NHS) celebrates its 75th anniversary, the nation has been reflecting on NHS accomplishments.
Public opinion is clear – we all want to maintain the right to free health care at the point of delivery1. However, with the increasing burden of chronic disease and the limitations of conventional medicine, it is time for change. Change that shifts the focus within the NHS to crucial preventative healthcare, and a model that provides patients with the resources needed to change their diet and lifestyle habits in promotion of health. There are simply not enough GP’s to tackle the burden of chronic disease. The incorporation of nutritional therapy into NHS primary care could revolutionise patient care and outcomes. One existing and untapped resource is the network of 3,000 BANT practitioners currently working outside the NHS.
BANT practitioners are Registered Nutritional Therapy Practitioners trained and qualified in clinical practice, who habitually support clients with diet, weight management, diabetes prevention and symptoms of diet-induced chronic disease that the NHS is struggling to manage. Registered Practitioners are registrants on a Professional Standards Authority for Health and Social Care (PSA) accredited register held by the Complementary and Natural Healthcare Council (CNHC) (see box below for further information) making them ideally placed to help bridge this NHS resource shortfall. This article passionately advocates for why BANT practitioners should be in NHS primary care, and why after 75 years their continued omission is inexplicable.
The Burden of Chronic Disease
Chronic diseases, such as Type 2 diabetes and metabolic syndrome, pose a significant threat to the future of the NHS, unless change is made and made soon. In the UK alone, it is estimated that over 15 million people are living with at least one chronic condition2. That is almost a quarter of the population!
The number of people living with diabetes in the UK has topped 5 million for the first time3. An estimated 64.3% of adults in England are now classified as overweight or obese4,5. The modifiable risk factors for both these conditions include diet and lifestyle. These diseases not only reduce the quality of life for individuals but also place a heavy burden on healthcare resources.
The current social annual cost of obesity in the UK is estimated to be around £58 billion, equivalent to around 3% of the 2020 UK GDP6. The reality is that conventional medicine has little to offer when it comes to chronic disease resolution based on its model of a pill for every ill. The College of Medicine’s Beyond Pills Campaign launched in 2022, called for urgent Government intervention on over-prescribing in the NHS.
Speaking at the Integrative and Personalised Medicine Congress in June, The College of Medicine Chair Dr Michael Dixon said: “Medicine, as we know it, is no longer affordable or sustainable. Nor is it able to curb the increase in obesity, mental health problems and most long-term diseases.”
The Limitations of the Conventional Medical Model
While the conventional medical model has undoubtedly made significant advancements in treating acute illnesses and emergencies, it typically falls short when it comes to managing chronic conditions. Standard treatments for chronic diseases often involve long-term medication use as illustrated above. This may alleviate some of the symptoms but is never without side effects.
They also frequently fail to achieve the goal of wellness. Anecdotal feedback gathered by BANT from GPs at a series of health industry events hints at widespread frustration at their inability to help their patients, coupled with an interest in and admiration for what nutrition practitioners do in clinical practice. GPs are increasingly wanting to train to deliver more nutritional advice.
The practicalities, however, are that GPs have an average 10-minute consultation time to deliver all their patient’s medical needs and this will never be enough to tackle the dietary and lifestyle components of chronic disease. So, whilst providing better nutrition training to GP’s might be considered a great long-term strategy, why not tap into the knowledge already existing in nutritional therapy consultation rooms across the country?
This presents an ideal opportunity for greater collaboration with PSA-accredited BANT nutrition practitioners and supports the argument to bring them into NHS primary care.
The Role of Diet and Lifestyle
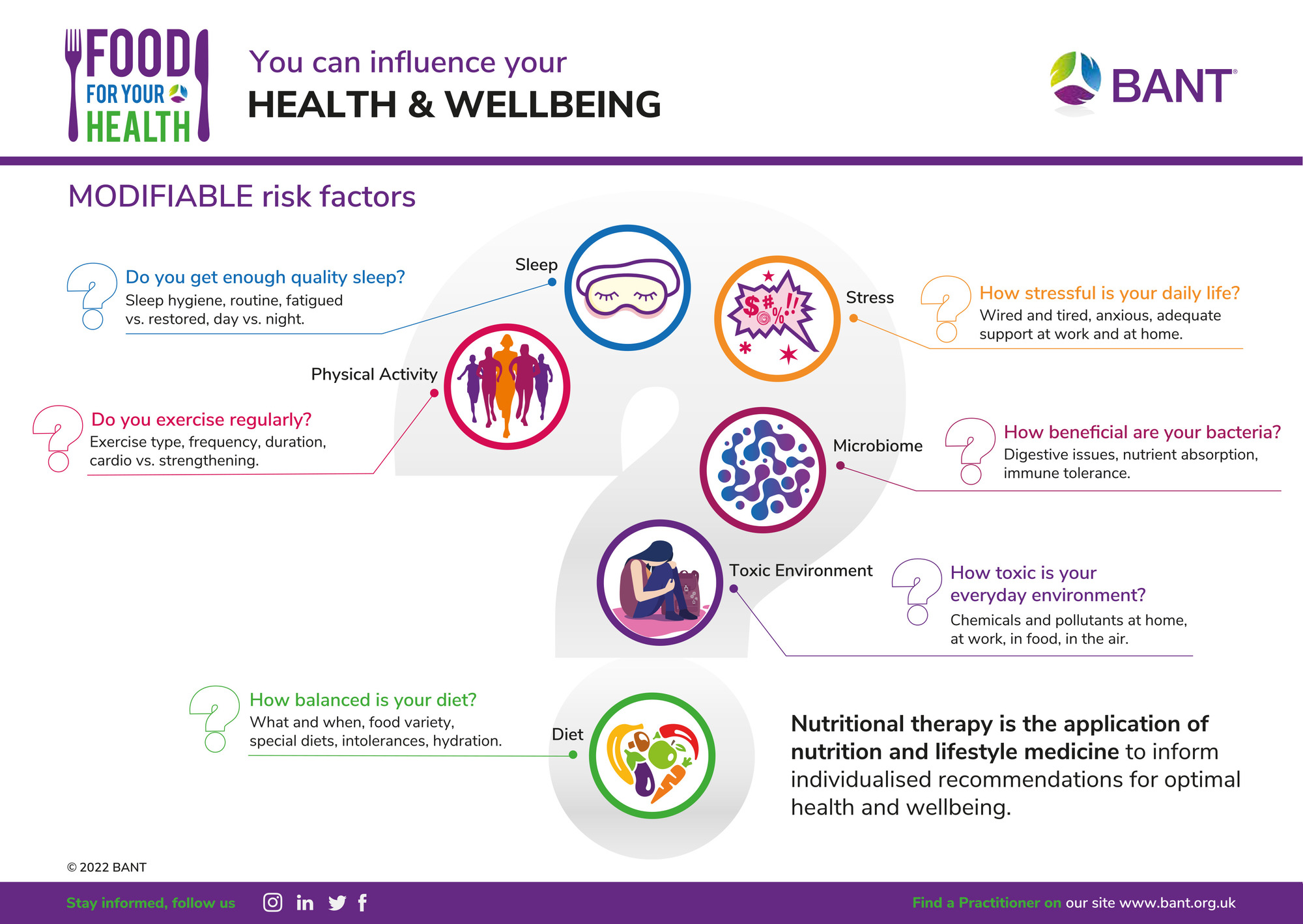
Research has shown that chronic diseases, such as Type 2 diabetes and metabolic syndrome, are closely linked to lifestyle factors, particularly diet (7,8). Modifiable lifestyle factors, including poor nutrition, physical inactivity, insufficient sleep, and chronic stress, contribute significantly to the development and progression of these conditions.
Recognising the impact of diet and lifestyle allows us to explore alternative approaches to care and prevention. One that puts the patient firmly in control of their health outcomes and supports them with the behavioural change necessary to modify their diet and lifestyle choices.
Modifiability of Chronic Disease with Diet and Lifestyle
Nutritional therapy and personalised nutrition focus on using food and dietary interventions to prevent risk-factors for chronic non-communicable disease and to optimise health. BANT nutrition practitioners adopt a personalised approach, getting to know their clients concerns and health goals and then helping them make sustainable, personalised changes to their diet and lifestyle.
They are clinically trained to do this and have the advantage of longer consultation times with clients, as compared to GPs, in which to support clients. The same principles have also been demonstrated in group sessions highlighting that the success of one-to-one interventions is scalable to better support public health.
BANT CEO, Satu Jackson and Director Isabel Hemmings recently presented findings from one such group program for diabetes prevention at the 2023 Integrative Personalised Medicine congress, demonstrating how participants recorded improvements across weight, BMI, waist circumference and mental health scores over the 12 week program. Numerous studies also demonstrate the profound impact of diet on managing and even reversing some previously intractable chronic diseases such as Type 2 Diabetes Mellitus9.
The Effectiveness of Nutritional Therapy
Nutritional therapy is a key part in managing “syndrome” conditions, such as metabolic syndrome, irritable bowel syndrome (IBS), fibromyalgia and chronic fatigue syndrome, polycystic ovary syndrome (PCOS) and many more. These conditions often lack a clear etiology and can be challenging to treat with conventional medicine which typically targets one symptom at a time, due to the complexities of interconnected symptoms.
By addressing the unique nutritional needs of each patient, BANT nutrition practitioners can offer effective strategies for managing symptoms and improving overall well-being. Practitioners routinely work with individuals who have complex symptoms or a dual diagnosis of one or more syndromes. If you would like to find out more about how BANT practitioners work or search for a practitioner visit bant.org.uk.
Why Registered Nutritional Therapy Practitioners should be in NHS Primary Care
Integrating Registered Nutritional Therapy Practitioners into NHS primary care could mean that in 25 years’ time, we will be ready to celebrate the 100th year of the NHS. It could be thriving once more, along with the UK population. Prevention is crucial, but the nation’s health crisis needs innovation not just investment.
Throwing money at an already broken NHS will solve very little. Similarly, asking already over-stretched GPs and healthcare workers to do more is unrealistic. We need to introduce new practitioners, with the correct skill set to address the burden of chronic disease. We need to empower patients to take an active role in their health by providing them with personalised dietary and lifestyle advice and support.
This can be done on both an individual basis and in groups. By integrating Registered Nutritional Therapy Practitioners into NHS primary care, there would be a dedicated workforce to provide preventative diet and lifestyle guidance, which in turn would help reduce reliance on medications and over-prescribing, and longer-term lead to better patient compliance and improved health outcomes. Leaving more time for doctors to do the job they trained for.
The Difference Between Registered Nutritional Therapy Practitioners and Dieticians
Only Registered Nutritional Therapy Practitioners and Registered Dietitians are trained and qualified in clinical practice to meet national standards and work in a one-to-one setting.
What differs between Registered Nutritional Therapy Practitioners, and Dietitians is the scope of practice. Both are trained in clinical skills. Dietitians are statutorily regulated health professionals that assess, diagnose, and treat dietary and nutritional problems typically within an acute care hospital setting.
Registered Nutritional Therapy Practitioners mostly work in the private preventative healthcare sector providing personalised dietary and lifestyle recommendations to optimise health and tackle the risk-factors for diet-induced chronic conditions. This is what GPs are asking for. This is what is needed in NHS primary care. Oftentimes, it is too late for prevention when a patient is admitted to hospital and gets seen by a Dietitian. When it comes to prevention we have the people-power trained, experienced and ready to go in the form of c. 3,000 PSA-accredited BANT practitioners.
More specifically, BANT practitioners combine a network approach to complex systems, incorporating the latest science from genetic, epigenetic, diet and nutrition research to inform individualised recommendations. BANT owns and runs a nutrition and lifestyle science database called Nutrition Evidence, the UK’s first scientific database of nutrition and lifestyle medicine research.
It focuses on high-quality, human research and other science-supported information and is designed as a comprehensive platform for practitioners, academic researchers, and students. The powerful, yet simple search functionality uses functional and lifestyle medicine filters to support evidence-based clinical decision making in personalised nutrition practice.
BANT membership requires min. of BSc (Hons) training in nutrition and lifestyle medicine sciences together with clinical training. To maintain their membership, members are required to meet Continuing Professional Development (CPD) Standards.
As the NHS celebrates its 75th anniversary, we can make one simple change. By recognising the modifiability of chronic diseases with diet and lifestyle interventions and embracing the effectiveness of nutritional therapy for chronic conditions, we can usher in a new era of patient-centred care within the NHS. This is why Registered Nutritional Therapy Practitioners should be in NHS primary care. Let’s get nutritional therapy out of private practice and the hands of the few, and into public health provision, available to all.
________________________________________
If you would like to know more about how changing your diet and lifestyle may impact your health, visit bant.org.uk and visit our free food for your health resources.
References:
1https://www.kingsfund.org.uk/publications/public-and-nhs-whats-the-deal
2https://www.kingsfund.org.uk/projects/time-think-differently/trends-disease-and-disability-long-term-conditions-multi-morbidity#:~:text=About%2015%20million%20people%20in,pulmonary%20disease%2C%20arthritis%20and%20hypertension.
3https://www.diabetes.org.uk/about_us/news/number-people-living-diabetes-uk-tops-5-million-first-time
4House of Commons Obesity Statistics January 2023 - https://researchbriefings.files.parliament.uk/documents/SN03336/SN03336.pdf
5https://www.healthexpress.co.uk/obesity-statistics-uk
6https://www.frontier-economics.com/uk/en/news-and-articles/articles/article-i9130-the-annual-social-cost-of-obesity-in-the-uk/#
7Effects of a lifestyle intervention on the biomarkers of oxidative stress in non-communicable diseases: A systematic review - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10034086/
8The effectiveness of diet intervention in improving the metabolism of overweight and obese women: a systematic review and meta-analysis - https://www.nutrition-evidence.com/article/35702099?term=35702099&limit=expert_opinion:Plain%20Language%20Summary
9Dietary Interventions to Treat Type 2 Diabetes in Adults with a Goal of Remission: An Expert Consensus Statement from the American College of Lifestyle - https://www.nutrition-evidence.com/article/0e02899c5654fb8b10a50f61b7a22e70
