Why NHS Junior Doctors Are Considering Going On Strike
The last time junior doctors went on strike was in 2016 (Alamy)
9 min read
Junior doctors in England are holding a ballot on industrial action that could see them walk out for 72 hours in March in the latest dispute over pay to hit the NHS workforce.
The possibility of a junior doctors' strike is the latest thread of widespread public sector disruption, with other NHS health workers, transport workers and possibly teachers walking out in the coming months.
Unions from multiple sectors are calling for pay rises as the cost of living crisis bites this winter, and with the NHS already under immense pressure, health worker strikes are likely to continue to dominate headlines.
Nurses are set to stage their third stoppage on 18 and 19 January while ambulance staff are due to refuse to work for a second and third time on 11 and 23 January.
Here is everything you need to know about the junior doctors' strike ballot…
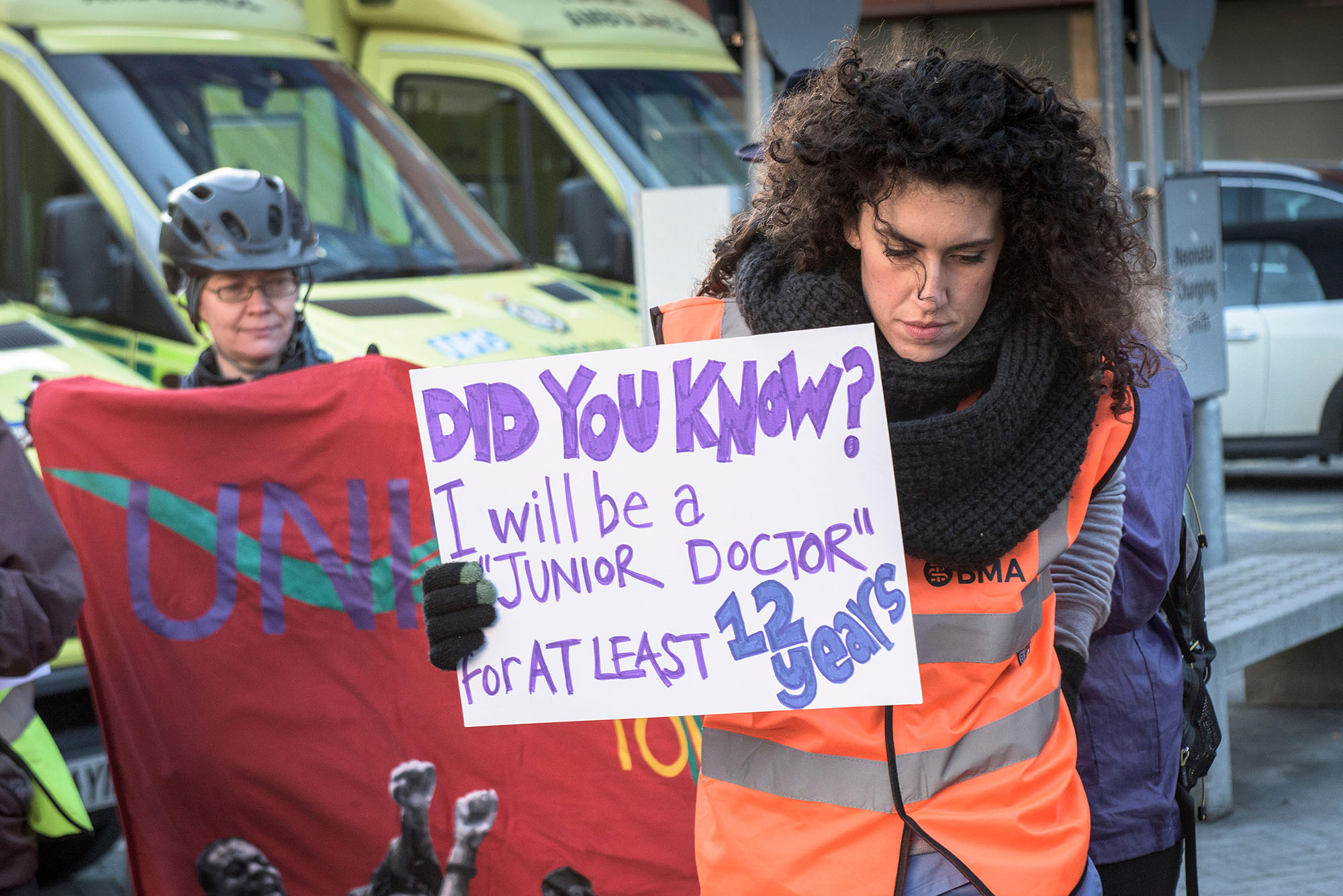
Who are junior doctors?
Junior doctors are qualified doctors in clinical training. They can have more than 10 years experience working as a hospital doctor or at least three years as a GP.
 Junior doctors make up almost half of all doctors in hospitals in England (Alamy)
Junior doctors make up almost half of all doctors in hospitals in England (Alamy)
Despite their “junior” title, junior doctors range from those who have just qualified (referred to as ‘F1s’ and ‘F2s’ in their first two years) to those with many years of medical experience.
Technically they are not yet qualified to practise independently without a supervising consultant responsible – but many junior doctors have said that under the current pressures facing the NHS, they are sometimes left feeling unsupported in charge of entire wards.
Junior doctors make up almost half of all doctors in hospitals in England – around 70,000 in total – and more than 45,000 junior doctors will be balloted to strike.
What is the background to the current dispute?
The last time junior doctors went on strike was in 2016, in protest over a new contract that unions said did not protect staff from being overworked.
In 2019, after a four-year dispute, the government agreed a new contract with junior doctors that saw them receive a pay rise averaging two per cent for each of the next four years, starting in 2020.
The contract also put new limits on weekend working and the number of night shifts they can do in a row.
What demands do junior doctors have now?
In 2023, the British Medical Association (BMA), the main trade union for doctors in the UK, is demanding “full pay restoration” for junior doctors.
The 2019 contract guaranteed junior doctors in England a two per cent pay rise in 2022/23, which 82 per cent of junior doctor members agreed to accept in a referendum voting on the contract, ending months of dispute at the time.
However, the union now argues that because the contract was written before the Covid-19 pandemic and when inflation was only at two per cent, it now needs reconsidering.
The BMA says that the contract agreement has a ‘betterment’ clause that allowed for exceptional circumstances to be considered when setting the rate of pay.
 The British Medical Association is the main trade union for doctors in the UK (Alamy)
The British Medical Association is the main trade union for doctors in the UK (Alamy)
Their calculations show that pay awards for junior doctors in England from 2008/09 to 2021/22 have delivered a real terms (RPI) pay cut of 26.1 per cent.
F1s are currently paid £14.09 per hour and the “full pay restoration” would see their pay increase to £18.69. In total, pay restoration for all junior doctors would have a net cost to the government of £1.03bn.
Since early 2022, the BMA’s Junior Doctors’ Committee (JDC) has escalated the campaign on pay to address long-term pay erosion faced by NHS doctors.
As well as pay rise demands, many junior doctors cite heavy workload and stressful conditions as reasons for voting to strike.
How has the government responded to the BMA’s demands?
The BMA is urging the government to meet with doctors and negotiate a solution to avert the strikes, but says Health Secretary Steve Barclay is “the first health secretary for over 50 years to continue to ignore all invitations from the BMA to meet with doctors, making attempts to find a negotiated settlement virtually impossible”.
The Department of Health and Social Care said: “Our multi-year pay deal with the British Medical Association is increasing junior doctor’s pay by a cumulative 8.2 per cent by 2023.
“We have also invested an additional £90m to provide the most experienced junior doctors with higher pay, increased allowances for those working the most frequently at weekends, and increased rates of pay for night shifts.”
Why are junior doctors voting to strike?
It is expected that a majority of BMA members will vote to strike.
Dr Martin Whyte, deputy chair of the BMA’s Junior Doctors’ Committee, graduated from Newcastle University in 2015 and now works in paediatrics as a registrar in the north east of England – the last stage of doctor training.
He argues that while junior doctors’ pay has not kept up with inflation, workload has increased year on year.
“More and more patients every year are coming with long-term illnesses,” Whyte said, an issue that has been exacerbated by the Covid-19 pandemic.
“The pay does not represent the level of skill needed to do the job,” he continued. “We want full pay restoration, we deserve that."
He also suggested that addressing the pay issue will help to solve the problems in the NHS with retaining staff. A BMA survey in December showed 40 per cent of junior doctors are actively planning to quit the NHS as soon as they can find another job.
Sophie Holmes, a 25-year-old F2 junior doctor at Southend University Hospital in Essex, has also decided to vote in favour of strike action because she feels the level of pay does not reflect the sacrifices young doctors have to make.
Holmes explained that most junior doctors have paid for up to six years of university fees, racking up debt in the process.
“Most will have worked jobs on the side to fund their studies whilst having to attend placements, lectures, and teaching – which can be the equivalent hours as a 9-5 job in itself,” she told PoliticsHome.
“When they finally graduate, they start on a salary that is barely enough to cover bills and begin a job that is physically and emotionally stressful.
“In any other sector, if you had 6 years of specialist training you would be earning so much more than a junior doctor does."
Describing an NHS “on its knees”, Holmes said she has never seen it as under pressure as it is now: “I wouldn't want a family member to be unwell and require urgent care right now because the standard of care we strive to provide is so hard to achieve in the current situation.
“I genuinely love my job, and I wouldn't change it for the world, but the environment and pay are making it hard to remember why I love it.”
An F1 junior doctor based in south London, who wished to remain anonymous, told PoliticsHome that she is having to do extra shifts to be able to afford rent, bills and a gym membership “to keep me sane”.
“The working conditions are unsafe,” she said. “We are so under-resourced and understaffed that it’s unsustainable for us to keep going like this.
“The emotional stress continues to take its toll on me out of the workplace. I do not feel my salary reflects the physical and mental battles I face to care for my patients.”
What would a junior doctor’s strike look like?
The ballot opens on 9 January and closes 20 February – and if the majority of voters choose to strike with at least a 50 per cent turnout, industrial action will likely take place in March.
If the strikes go ahead, the BMA will withdraw their labour from all NHS services, including emergency care, for three days – causing major disruption in hospitals and other services, including surgery and outpatient appointments.
NHS trusts would have to scale back services, and consultants would be redeployed to cover the work of junior doctors.
“This will have a huge impact and is very inefficient,” Whyte admitted, but added that the BMA would always give two weeks notice for strike action.
This disruption would coincide with a record 7.21 million people already waiting for NHS treatment in England.
Miriam Deakin, the director of policy at hospitals body NHS Providers, told The Guardian that the possible strikes are “deeply worrying” but that “trust leaders will do everything they can to minimise disruption and prioritise the safe delivery of care and services for patients”.
“Trust leaders are very concerned about the possibility of prolonged or coordinated strike action by health unions in the coming months,” she said.
“They also understand the factors that have driven junior doctors and other healthcare workers to ballot on industrial action.”
